OUR STORY
We fixed the problem years ago
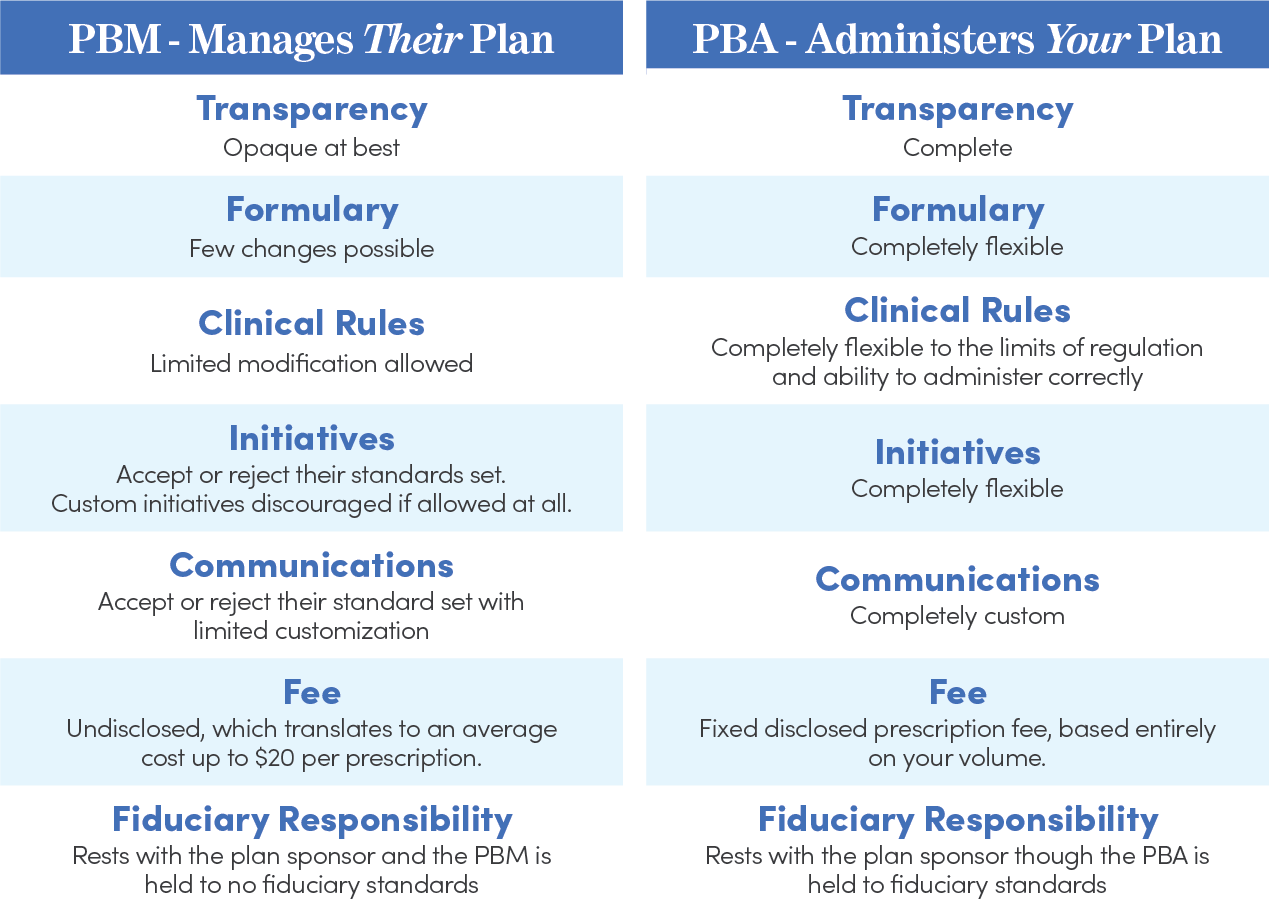
We broke free from the traditional vague and unaccountable PBM model almost twenty years ago when we realized the PBM was becoming more a part of the problem than the solution.
It started in 2001 when a large health system approached our founder, Creelgroup Consulting, with a problem. Their Pharmacy plan costs were going up 12% a year and the major international consulting firm the relied on was telling them they were performing at an excellent level. As a Health System they had direct knowledge of true drug prices and therapeutic uses which made them think something had to be wrong costs should not be going up this fast. We spent months doing a deep dive into the world or pharmacy contracts, rebates, indirect reimbursements, and formulary steerage and agreed something was wrong and we knew how to fix it.
THE SOLUTION
We Created a New Type of Pharmacy Plan
- We replaced the Pharmacy Benefit Manager (PBM) model replaced with a new Pharmacy Benefit Administrator (PBA) model
- We contracted to ensure the PBA could receive no income other than the fixed fee paid directly by the client
- We created a formulary incentivizing the use of the most cost effective and clinically effective therapies not the ones providing the biggest rebates
- We contracted to ensure full true transparency — all contracts including rebate contracts had to be available to audit
- We contracted to ensure 100% true pass-through pricing with no spread pricing and no direct or indirect fees flowing back to the PBA through charges to the pharmacy
- We contracted for Performance guarantees and penalties based on absolute measures of improvement
- We implemented a Pharmacy plan that established annual targets for improvement and implemented specific initiatives each year to ensure targets were met
THE RESULTS
Lower costs at every level
- Moving to our model from the PBM model cost typically reduces 15% to 20% with no cost transference to the member.
- Plans maintains maintain their low cost with no mandatory generics, no mandatory or heavily incentivized mail order and an open formulary design with all FDA-approved drugs covered when used for FDA approved purposes